Lactose, a disaccharide composed of galactose and glucose, is the main sugar derived from milk. Lactose is present in a wide range of food products but is also used in the pharmaceutical industry as an excipient.
Once ingested, the digestion of the lactose normally consists in 3 majors steps:
- Digestion begins in the mouth, with the help of the mastication mechanism and the enzymes that are released.
- Then, in the small intestine, lactose is split into two molecules that are then converted into energy. This splitting process occurs thanks to a specific enzyme: lactase.
- Finally, in the large intestine, lactose is digested via the microbiota. Most lactose is digested, there, when lactase is observed to be deficient.
The inability of the body to properly digest lactose can sometimes lead to certain discomfort (diarrhea flatulence and abdominal pain), often called lactose intolerance.
But what is lactose intolerance? Is it an issue to consider when formulating medications?
Lactose intolerance: origins and consequences
What is lactose intolerance and what are its consequences?
Some people are unable to digest lactose or have difficulties digesting it. It is in reference to such cases that we use the term lactose intolerance. Lactose is poorly digested and causes gas to be produced in the large intestine (H2, CO2, CH4) and water to be drawn up, resulting from the production of fatty acid chains. It induces diarrhea, bloating, flatulence and abdominal pain. However, it is important to distinguish lactose intolerance from allergies, which can cause allergic reactions, rashes or respiratory problems. For example, Cow’s Milk Protein Allergy (CMPA) [AB1] can be particularly serious, especially for children. In fact, CMPA is the main pediatric allergy. Let’s now see how the digestion of lactose works in the human body.
Digestion in the small intestine
Digestion in the small intestine requires the production of a specific enzyme: lactase. The digestion process can be impacted in three different ways.
Firstly, a temporary intolerance, such as an intestinal inflammation or infection, can lead to the body being unable to produce lactase for a certain period of time. This is known as secondary lactase deficiency.
Secondly, it can manifest as an acquired primary deficiency. If an individual does not have the “lactose persistence gene”, lactase production is reduced during their lifetime, especially in adulthood. It is quite usual in mammals, as they consume less milk as adults. Over time, human populations have lost the ability to digest lactose, because milk was either not consumed or consumed infrequently. In human adulthood, 70% of people no longer produce enough lactase in order to properly digest the lactose contained in milk.[1] Often, Caucasian populations in Northern Europe are lactose persistent because they have regularly consumed cow’s milk as a result of the domestication of cows.
Finally, the non-digestion of lactose in the small intestine can be due to a congenital lactase deficiency. It means that the body is unable to synthesize lactase.
Digestion in the large intestine via the microbiota
Lactose not fully digested in the small intestine, arrives intact in the colon, where the local microbiota adapts to the substrate provided by the diet. Lactose is therefore a source of energy for the intestinal bacteria. Lactose also modifies the composition of the intestinal microbiota and even has a potential prebiotic effect in the large intestine. Never fully hydrolysed in the small intestine, even for people that produce lactase, lactose plays an important role in the maturity of the microbiota in the large intestine, enabling certain important strains to develop like bifidobacteria. It is particularly beneficial in the first few years of life.[1] In regard to the effect of lactose consumption on the microbiota, it is therefore possible that an imbalance in its composition may be a cause of intolerance.[2]
Lactose intolerance in the pharmaceutical industry
Pharmaceutical lactose[AB1]
Lactose is derived from milk and is widely used in the pharmaceutical industry as an excipient. Currently, it is present in almost 60% to 70% of Oral Solid Doses. The success of lactose is due to its qualities: its neutrality, high purity and absence of reaction with the active ingredient, ensuring its safety, its accessibility, its physiochemical properties and finally, its versatility. In pharmaceuticals, lactose is considered as a safe excipient, with limited negative interactions with drugs. A medicine, tablet or capsule, contains between 0,1 g to 0,2 g of lactose, i.e., around 63 times less than a 250 ml glass of milk that contains around 12.6 g of lactose.
Lactose intolerance in pharmaceuticals: a non-existent problem?
In the pharmaceutical industry, lactose is used in low doses. According to medical research, there are no symptoms of intolerance for most individuals, if between 6 to 12 g of lactose per day are ingested, in patients who do not express lactase.[1] However, there may be a wide variation in the tolerance threshold between patients. But in the case of pharmaceuticals, concerns of this nature are unfounded, because intakes do not reach such orders of magnitude. For example, with two tablets containing lactose as excipient, the lactose quantity delivered is between 0.2 and 1.4 mg.[2]
Pharma processes can influence the speed at which lactose becomes available in the intestine, but on a reduced scale. Furthermore, its capacity to be digested is not altered because the structure of lactose remains the same, whatever its form (i.e., monohydrate or anhydrous).
However, as lactose is considered as an “excipient with a known action or effect” [AB1] by the European Union, its presence in medicinal products must be mentioned in the package leaflet.[1]
Besides, to avoid any risk, some medicines are specifically formulated without lactose. For example, this is the case with the Levothyrox medicines. Their formulas were changed by the Merck Laboratory in 2017, in part to remove lactose.[2]
To conclude, lactose intolerance can be a source of discomfort in terms of digestion, food choices and intake requirements. In pharmaceuticals, lactose is used as an excipient, but the doses used are so low that problems of lactose intolerance do not arise. Nevertheless, lactose is mentioned on the package leaflet of medicines, and alternatives such as mannitol exist, to avoid any risk.*
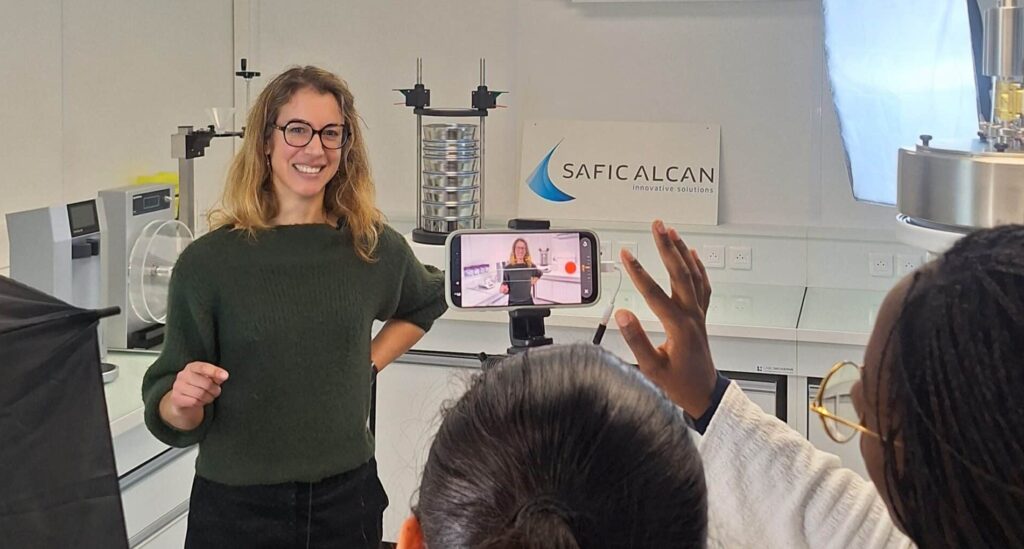
To learn more about lactose intolerance and many other topics, you can watch the replay of our expert-led webinar, entitled “Is lactose still an underrated sugar or a health ally?”. Take this opportunity to discover the scientific aspects of lactose and how does it differ from other sugars, as well as its surprising health and nutritional benefits!
[1] https://www.ema.europa.eu/en/human-regulatory-overview/marketing-authorisation/product-information-requirements/excipients-labelling
[2] https://www.vidal.fr/actualites/21946-levothyrox-precisions-et-actions-suite-aux-inquietudes-et-plaintes-de-certains-utilisateurs.html
[1] Misselwitz, Benjamin, et al. “Lactose malabsorption and intolerance: pathogenesis, diagnosis and treatment.” United European gastroenterology journal 1.3 (2013): 151-159.
[2] Paques, Marcel & Lindner, Cordula. (2023). Lactose: Evolutionary Role, Health Effects and Applications.. 10.1016/C2016-0-00999-3.
[AB1]Lien interne lactose as an excipient : The benefits of lactose as an excipient – Lactalis Ingredients Pharma
[1] Guerville, M. Ligneul, A. (2024). « Le lactose : un sucre pas comme les autres. Lactose: a sugar like no other. Cahiers de Nutrition et de Diététique volume 59 issue .2023.12.004
[2] Francavilla, Ruggiero, et al. “Effect of lactose on gut microbiota and metabolome of infants with cow’s milk allergy.” Pediatric allergy and immunology 23.5 (2012): 420-427.
[1] https://cdhf.ca/fr/what-is-lactose-intolerance-symptoms-and-treatment/;
Gerbault, Pascale, et al. “Evolution of lactase persistence: an example of human niche construction.” Philosophical Transactions of the Royal Society B: Biological Sciences 366.1566 (2011): 863-877.
[AB1]Lien article APLV : CMPA and lactose intolerance in infants – Lactalis Ingredients